What Clinical Metrics Miss About Patient Safety and Equity
From a hospital bed with a serious illness, I witnessed what healthcare metrics often overlook. As a cancer survivor and systems design expert, I began to notice how well-meaning systems can quietly fail—unseen errors, overlooked risks, and preventable harm that slip silently through the cracks of daily care.
What’s troubling is that these failures occur even when everything appears to be in order—by the chart, the protocol, or the performance metric.
That realization changed the course of my life. I pivoted my career from tech to healthcare innovation—not for personal gain, but to help others avoid the preventable harm I experienced. Through a multi-year research grant and collaboration with clinicians at a leading academic medical center, I developed new methods to turn lived experience into operational intelligence. This approach uncovers hidden safety risks—enabling providers to spot patterns they hadn't seen before.
Most healthcare professionals haven’t experienced a life-threatening illness personally. Most patients haven’t studied systems design. That dual perspective helped me identify hidden failures that neither viewpoint could fully detect on its own.
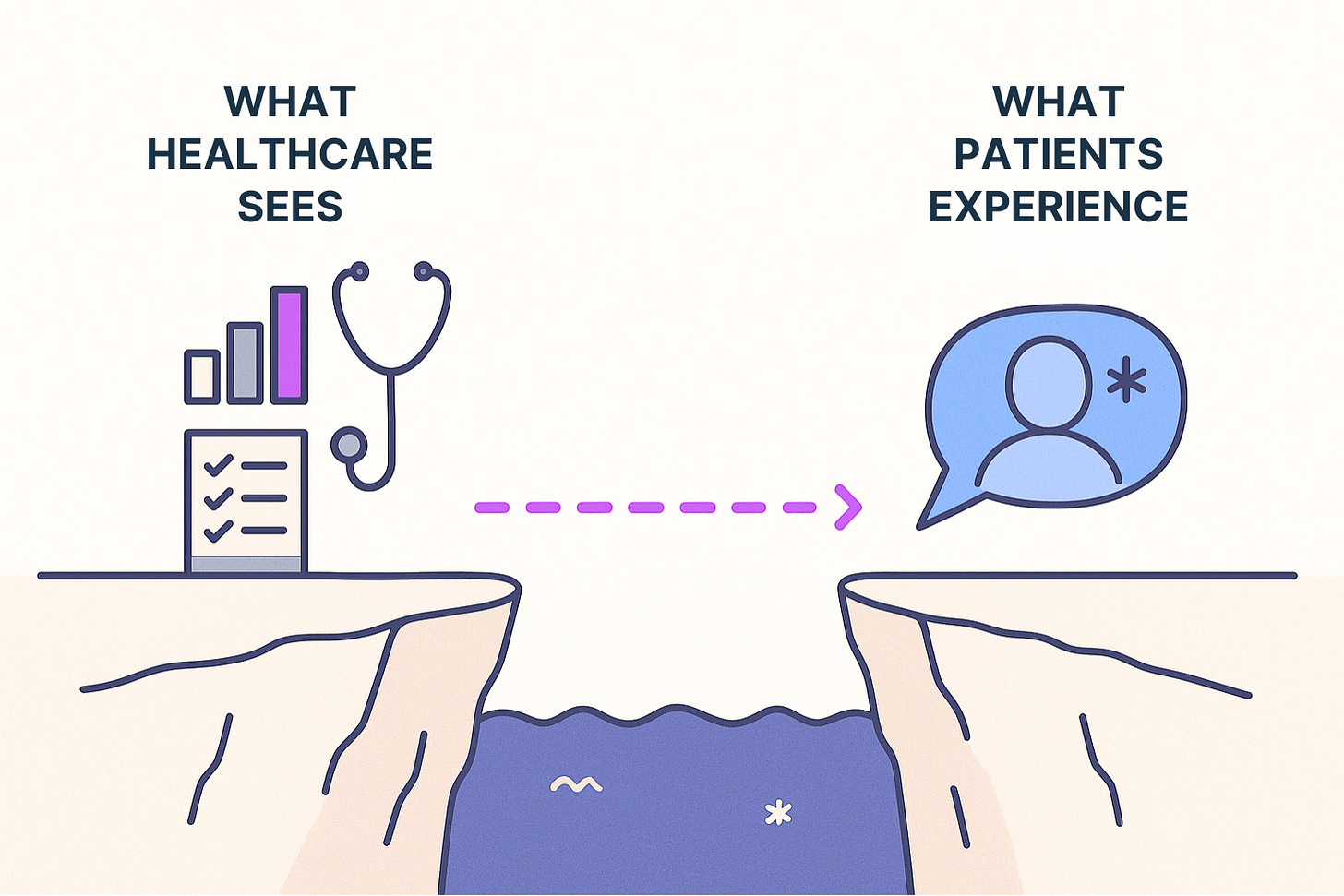
The Gap that Hides Risks
Patient advocacy raises awareness and influences policy. Clinical research underpins evidence-based practice. Quality metrics measure performance and inform improvements. Yet despite decades of effort, safety breaches and system failures continue. Why?
Each of these disciplines operates in a silo. They generate essential data, but they don’t integrate patient experience into the system's inner workings. Clinical research and quality frameworks are built around data observable by providers, not the lived experiences of patients—as they navigate care. As a result, they often miss warning signs that patients feel but providers cannot see
This explains why providers sometimes receive patient complaints that seem illogical or why safety issues persist despite protocols being followed. These are often not individual provider failures—they’re consequences of a system that lacks insight into how care truly happens at the bedside.
The Missing Bridge Between Patient Experience and System Learning
That’s the kind of visibility I was trained to create.
In human-centered design, the field where I honed my skills, we use observation, empathic interviews, contextual inquiry, and systems mapping to uncover patterns, signs of confusion, friction points, and hidden risks. We examine lived experiences to generate insights that guide design—delving deeper than traditional patient surveys to understand unarticulated and underlying issues.
That lens doesn’t seem to be systematically applied to clinical care. At the top academic medical center where I received care—with a well-resourced patient experience department—I still encountered serious safety gaps. These weren’t isolated missteps, but signs of a deeper problem: the absence of a structured, design-informed methodology for interpreting lived patient experience at the bedside.
Without that kind of analysis, even well-intentioned systems remain blind to the risks they inadvertently create.
So I developed one—a methodology that bridges lived experience and system learning.
Introducing Ask the Patient
I created Ask the Patient to provide a new kind of patient experience insights: bedside intelligence. What sets Ask the Patient apart is its integration of patient experience with systems design to uncover how risks and failures develop—and remain hidden—at the point of care. This approach reveals not just what goes wrong, but why.
Beginning with my own healthcare journey and extending to those of other patients, I use experiential system analysis—a method that applies structured investigation to uncover system patterns and behaviors embedded in lived experiences. Clinicians found the results eye-opening in a pilot program. It is, in essence, a system analysis of healthcare delivery from the inside out—an approach that hasn't been applied to clinical care before.
Why This Matters Now
Despite decades of patient-centered efforts and billions of dollars invested in healthcare improvement, safety breakdowns, health inequities, provider burnout, and public mistrust persist. My dual perspective as both a patient and a systems expert revealed a critical disconnect: healthcare lacks visibility into the lived patient experience, making it difficult to fully understand what issues are problematic.
Without this visibility, healthcare treats these persistent challenges as separate problems to solve in isolation. This veil obscures the common thread connecting these ongoing challenges—preventing healthcare from addressing their shared root cause.
Patient experience holds essential intelligence needed to solve these issues, but it remains hidden in a form that healthcare systems don't know how to access.
Key insights about operational failures and inequities stay buried in patient journeys, and traditional metrics cannot measure them.
New methods are needed to extract operational intelligence from lived experiences.
This was my personal experience at a leading academic hospital: my biopsy results were lost, my cancer was missed and misdiagnosed, and I was seriously harmed during a medical procedure with life-threatening complications—yet clinicians never recognized that something was wrong or that harm occurred. Friends encouraged me to take legal action, but I chose a different approach: using my experience to help health systems prevent these failures—rather than retaliating and helping nobody.
This is why Ask the Patient was born—as a way to fill this visibility gap. By combining system design expertise with patient experience insights, we can develop a deeper, more actionable understanding of how to make care safer, more equitable, and more effective.
Patient experiences contain untapped insights to improve healthcare delivery. "Ask the Patient" extracts and delivers these insights directly to you. Whether you're a healthcare professional seeking to enhance safety and outcomes or a patient seeking to drive systemic change, “Ask the Patient” provides the insights you need. Like, share, and comment if this post resonates.



Nice work, Sylvie! This is really beautiful. Healthcare is incredibly siloed. The more we can connect and learn the perspectives of others, the better we’ll understand the system, support those harmed by it, and provide a restorative response.
Patients are experts and have so much to teach us all. Designing systems to bring patients and providers together in truly authentic ways (not just to check a box) will help a lot!!
Thank you for being vulnerable and sharing your voice. This post is proof. You’ve taught us all!
Perhaps we need on call patient consultants in healthcare?
Sylvie, this is such a crisp and clear explanation of why “Patient Experience” has never been just about surveys and why experience is a leadership responsibility, not a department.
Your insight about patient experience as intelligence rather than evaluation resonates. The most adaptive organizations I’ve worked with treat patient feedback as system data not just satisfaction scores to react to, but signals to design around.
Thank you for reframing experience as integral to performance, improvement, and culture. We need more voices pushing for this kind of integration.